Cancer's recruitment drive of healthy cells targeted
2012-11-21 06:35:50
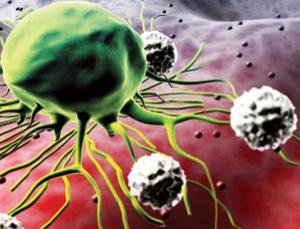
FUTURE treatments for breast cancer may include an unusual target - perfectly
healthy cells. The idea is to prevent cancer cells from recruiting healthy cells
to help them grow and spread.
Two new strategies to stop this kind of collusion in breast cancer were
presented at the annual conference of the National Cancer Research Institute in
Liverpool, UK, last week. One would forestall the dampening of the immune system
after cancer treatment, that seems to allow surviving tumour cells to
proliferate. The other would stop breast cancer reaching organs like the lungs
by blocking an accomplice vital to any such spread.
The first strategy would mean that women who have already had treatment for
breast cancer would take an additional course of a cheap, relatively non-toxic
anti-cancer drug, cyclophosphamide. A study of 35 women showed that the drug
might prevent cancer relapses by reducing levels of regulatory T-cells which
suppress the immune system. These cells are more common in women with
particularly large and aggressive breast cancers.
"If you use cyclophosphamide at low doses, you can reduce [numbers of these
cells] substantially without affecting other cancer defences," says Oleg Eremin
of the Queen's Medical Centre at the University of Nottingham, UK.
Eremin got the idea of using cyclophosphamide by tracking levels of regulatory
T-cells in women with breast cancer before, during and after treatment. All the
women had large breast tumours and some had six times the normal level of the
T-cells. This suggested that the cancer cells somehow ramp up the number of
their "accomplices".
After shrinking the tumours with chemotherapy, which included cyclophosphamide
alongside two other drugs, then surgically removing any tumours still present,
Eremin's team found that the women's regulatory T-cell counts fell substantially
but remained above normal. They also began to creep up again once the
chemotherapy had ended. His hunch is that resistant cancer cells might linger in
the body and stimulate the production of the T-cells.
Before probing whether a second course of cyclophosphamide can stop this and so
help prevent relapses, Eremin hopes to follow the same women for at least six
months to see whether their regulatory T-cell counts keep rising. If so, this
would reinforce the rationale for attempting to keep these cells in check with
cyclophosphamide, he says.
Meanwhile, Clare Isacke and her colleagues at the Institute of Cancer Research
in London have made headway in the battle to prevent breast cancer cells from
spreading into the lungs, liver and other tissues.
The process begins with the cancer cells binding to the surface of blood vessels
in the lungs. Isacke has discovered that the cells can only do this if they
attach to a protein "accomplice" in the blood, and that this binding can
potentially be blocked with drugs.
Isacke also found that cancer cells were least invasive if they lacked the
surface sugars indispensable for grasping the protein. Blocking the protein,
which she will name when she publishes her results in full, might be enough to
reduce cancer's spread, and Isacke is confident drugs can be found that do this.
"We'd like to find ways to disrupt this collusion without harming normal
interactions between healthy cells," she says.
Comments